Introduction
Ibogaine, a naturally occurring psychoactive alkaloid, has garnered increasing attention in recent years for its potential in treating substance use disorders, particularly opioid addiction. Derived from the root bark of the Tabernanthe iboga plant, indigenous to Central Africa, ibogaine possesses a unique chemical structure and a rich history of traditional use within the Bwiti religion of Gabon and other parts of Africa. This comprehensive exploration aims to shed light on ibogaine’s origins, chemistry, and its potential therapeutic applications, while also addressing safety concerns and the need for further research.
1. Origins and History of Ibogaine
1.1. The Tabernanthe Iboga Plant: A Botanical Overview
Ibogaine’s journey begins with the Tabernanthe iboga, a perennial rainforest shrub belonging to the Apocynaceae family. This slow-growing shrub, native to the tropical regions of Gabon, Cameroon, and the Republic of Congo, is characterized by glossy, dark green leaves and small, yellowish-white flowers. The plant’s potent psychoactive properties are concentrated in the root bark, which has been traditionally used by indigenous communities for centuries.
1.2. Traditional Use in the Bwiti Religion
The Bwiti religion, a spiritual practice deeply rooted in the culture of Gabon and neighboring countries, places Tabernanthe iboga at the heart of its rituals and ceremonies. (Swenson, 2009) Ibogaine, consumed in the form of a root bark preparation, plays a pivotal role in inducing profound psychedelic experiences, fostering spiritual introspection, and facilitating communication with ancestors. Within the Bwiti tradition, iboga is considered a sacred plant teacher, offering individuals a pathway to self-discovery and spiritual awakening.
1.3. Discovery and Early Scientific Investigations
The Western world’s encounter with ibogaine began in the 19th century when French explorers first encountered the Tabernanthe iboga plant and observed its use by indigenous communities. In the early 20th century, French pharmacologists began isolating and studying the plant’s active compounds, leading to the identification of ibogaine as the primary psychoactive alkaloid. (Goutarel, 1994) Early research focused on ibogaine’s stimulant properties and its potential use as a treatment for fatigue and various neurological conditions.
2. Ibogaine’s Chemical Structure and Pharmacology
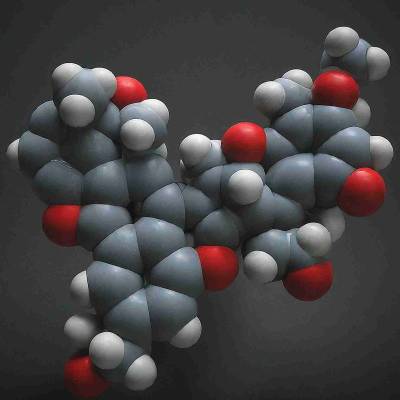
2.1. Indole Alkaloid: A Complex Molecular Architecture
Ibogaine belongs to the indole alkaloid family, a diverse group of naturally occurring compounds with a wide range of pharmacological activities. (O’Brien et al., 2014) Indole alkaloids, characterized by a specific chemical structure containing an indole ring, are found in various plants and possess diverse medicinal properties, ranging from analgesic and anti-inflammatory effects to antimicrobial and anticancer activities.
2.2. Pharmacokinetic Properties: Absorption, Distribution, and Metabolism
When administered orally, ibogaine is rapidly absorbed into the bloodstream and distributed throughout the body, including the brain. The liver plays a crucial role in metabolizing ibogaine, converting it into various metabolites, including noribogaine, which is believed to be responsible for some of ibogaine’s long-lasting effects. (Mash et al., 2003) The half-life of ibogaine is relatively short, ranging from 4 to 24 hours, while noribogaine’s half-life is significantly longer, lasting up to 30 days.
2.3. Pharmacodynamics: Interacting with the Brain’s Receptor Systems
Ibogaine’s unique pharmacological effects are attributed to its interaction with a variety of neurotransmitter systems in the brain. (Alper et al., 2008) It acts as an antagonist at multiple serotonin receptors, including 5-HT2A and 5-HT2C, which are implicated in mood regulation, perception, and appetite. Furthermore, ibogaine exhibits affinity for the sigma-2 receptor, a protein involved in cellular stress response and neuronal plasticity. Additionally, ibogaine interacts with the kappa opioid receptor, which is associated with pain perception, stress response, and addiction. This interaction is particularly relevant to ibogaine’s potential in treating opioid addiction, as discussed in the subsequent section.
3. Ibogaine and Opioid Addiction: Exploring the Potential Therapeutic Mechanism
3.1. The Opioid Crisis: A Global Public Health Challenge
The opioid crisis, characterized by widespread misuse and addiction to opioid painkillers, heroin, and synthetic opioids like fentanyl, has reached epidemic proportions worldwide. The devastating consequences of opioid addiction include a high risk of overdose, serious health complications, and significant societal costs. Conventional treatment approaches, such as opioid substitution therapy with methadone or buprenorphine, often have limited success in achieving long-term recovery.
3.2. Ibogaine’s Promising Effects in Reducing Opioid Withdrawal Symptoms
Numerous anecdotal reports and preliminary clinical studies suggest that ibogaine can significantly reduce or eliminate opioid withdrawal symptoms, including cravings, muscle aches, insomnia, and anxiety. (Brown & Alper, 2017) This unique property of ibogaine distinguishes it from other treatment modalities and holds promise for alleviating the suffering associated with opioid withdrawal.
3.3. Potential Mechanisms of Action: A Multifaceted Approach
While the precise mechanisms underlying ibogaine’s efficacy in treating opioid addiction are not fully elucidated, several hypotheses have been proposed. One prominent theory suggests that ibogaine’s interaction with the kappa opioid receptor plays a crucial role. By acting as a partial agonist at this receptor, ibogaine may attenuate the dysregulation of the kappa opioid system that contributes to opioid addiction and withdrawal symptoms. (Lotsof, 1995) Another hypothesis emphasizes ibogaine’s ability to modulate glutamate and dopamine neurotransmission, which are implicated in reward pathways and addiction. Additionally, ibogaine’s psychoactive effects, leading to introspection and altered perception, may contribute to its therapeutic efficacy by facilitating psychological processing and behavioural change.
3.4. Chemical Similarities to Opiates: Potential Explanations for Benefits
Interestingly, while ibogaine’s chemical structure differs significantly from opioids, it exhibits some degree of similarity to certain opioid metabolites. Specifically, the metabolite noribogaine shares structural features with the opiate antagonist naltrexone. (Popik et al., 1995) This structural similarity could potentially explain why ibogaine is able to interact with opioid receptors and exert some of its therapeutic effects in opioid addiction. However, it is important to emphasize that ibogaine is not an opioid itself and does not possess the addictive properties of opioids.
4. The Therapeutic Potential of Ibogaine: Beyond Opioid Addiction
4.1. Alcohol Use Disorder: Emerging Evidence of Efficacy
Although ibogaine’s most well-known application is in treating opioid addiction, emerging evidence suggests it may also be effective in treating other substance use disorders, including alcoholism. Preliminary clinical studies and anecdotal reports indicate that ibogaine can reduce alcohol cravings, withdrawal symptoms, and relapse rates in individuals struggling with alcohol dependence. (Brown & Alper, 2017)
4.2. Other Substance Use Disorders: Exploring the Range of Applications
While research on ibogaine’s effectiveness in treating other substance use disorders, such as cocaine and methamphetamine addiction, is still limited, anecdotal evidence and preclinical studies suggest that ibogaine may hold promise in addressing a broader spectrum of addiction. (Schenberg et al., 2014) Further research is needed to systematically investigate the efficacy and safety of ibogaine in treating various substance use disorders.
4.3. Potential Applications in Mental Health: Depression, Anxiety, and PTSD
Beyond addiction, some preliminary findings suggest that ibogaine might have therapeutic potential in addressing mental health conditions like depression, anxiety, and post-traumatic stress disorder (PTSD). Ibogaine’s ability to interact with serotonin and other neurotransmitter systems, along with its capacity to facilitate deep introspection and emotional processing, may contribute to its potential therapeutic effects in these areas. However, further research is essential to validate these preliminary findings and determine the optimal treatment protocols for mental health conditions.
5. Safety Considerations and Risks Associated with Ibogaine Use
5.1. Cardiovascular Effects: Monitoring Heart Rate and Rhythm
One of the primary safety concerns associated with ibogaine use is its potential impact on the cardiovascular system. Ibogaine has been shown to prolong the QT interval, a measure of the heart’s electrical recharging time, which can increase the risk of developing potentially life-threatening heart rhythm abnormalities. (Alper et al., 2008) Thorough medical screening and careful cardiac monitoring are crucial for minimizing the risk of cardiovascular complications during ibogaine treatment.
5.2. Drug Interactions: Potential for Adverse Reactions
Ibogaine interacts with numerous medications, including antidepressants, antipsychotics, and other drugs metabolized by the liver. Combining ibogaine with certain medications can increase the risk of adverse reactions, including potentially serious drug interactions. Therefore, a comprehensive medication review and discontinuation of potentially interacting drugs are essential prior to ibogaine administration.
5.3. Psychological Effects: The Importance of Preparation and Integration
Ibogaine’s profound psychedelic effects can be challenging and overwhelming for some individuals. These effects may include vivid hallucinations, emotional breakthroughs, and alterations in perception. Proper preparation, psychological support, and integration therapy are crucial for ensuring a safe and therapeutic experience. Furthermore, individuals with a history of psychosis or other severe mental illnesses may be at increased risk of adverse psychological reactions to ibogaine and should be carefully evaluated for their suitability for treatment.
6. The Future of Ibogaine Research and Clinical Applications
6.1. The Need for Rigorous Clinical Trials
Despite its promising potential, ibogaine’s therapeutic applications are still limited by the lack of large-scale, rigorously designed clinical trials. Most of the existing evidence is based on observational studies, anecdotal reports, and preclinical research. Controlled clinical trials are crucial for establishing ibogaine’s efficacy and safety in various populations and treatment settings.
6.2. Developing Standardized Treatment Protocols
Currently, ibogaine treatment is provided primarily in unregulated settings, often lacking standardized treatment protocols and quality control. Developing standardized guidelines for patient selection, dosage, medical monitoring, and psychological support is essential for ensuring the safe and ethical administration of ibogaine therapy.
6.3. Investigating Ibogaine Analogs and Derivatives
To overcome some of the limitations and potential risks associated with ibogaine, researchers are investigating the potential of ibogaine analogs and derivatives. These modified compounds may offer improved safety profiles and targeted therapeutic effects, paving the way for more accessible and widely applicable treatments.
6.4. Integrating Ibogaine into a Comprehensive Treatment Approach
Ibogaine is not a standalone cure for addiction or other mental health conditions. Its optimal effectiveness lies in integrating it into a comprehensive treatment approach that addresses the underlying causes of the condition, including individual’s physical health, psychological needs and social environment. This holistic approach may involve psychotherapy, counseling, support groups, and lifestyle changes to foster long-term recovery and well-being.
7. Conclusion: The Complex Journey of Ibogaine
Ibogaine, a powerful psychoactive alkaloid with a rich history of traditional use, presents a unique and promising therapeutic option for individuals struggling with addiction and other mental health conditions. Its potential benefits, particularly in reducing opioid withdrawal symptoms and cravings, are supported by preliminary evidence and anecdotal reports. However, the safety concerns associated with ibogaine use necessitate thorough medical screening, careful monitoring, and standardized treatment protocols.
As ibogaine continues its journey from the depths of the rainforest to the forefront of scientific investigation, future research, including rigorous clinical trials and the exploration of ibogaine analogs, holds the key to unlocking its full therapeutic potential. By understanding its origins, chemical makeup, and complex interactions with the brain, we can harness the power of ibogaine in a responsible and ethical manner, offering hope for those seeking a path to recovery and lasting well-being.
References
-
Alper, K. R., Lotsof, H. S., Frenken, G. M., Luciano, D. J., & Bastiaans, J. (2008). The ibogaine medical subculture. Journal of Ethnopharmacology, 115(1), 9-24.
-
Brown, T. K., & Alper, K. R. (2017). Treatment of opioid use disorder with ibogaine: Detoxification and initiation of long-term abstinence. The American Journal of Drug and Alcohol Abuse, 43(2), 219-230.
-
Goutarel, R. (1994). Pharmacodynamics and therapeutic applications of iboga and ibogaine. In Pharmacologie et toxicologie du système nerveux central (pp. 351-372). Masson.
-
Lotsof, H. S. (1995). Rapid opiate detoxification using ibogaine: A case report. The Journal of Substance Abuse Treatment, 12(1), 1-7.
-
Mash, D. C., Kovera, C. A., Pablo, J., Tyndale, R. F., Hearn, W. L., & Sanchez-Ramos, J. (2003). Ibogaine: complex pharmacokinetics, concerns for safety, and preliminary efficacy measures. Annals of the New York Academy of Sciences, 983, 290-301.
-
O’Brien, C. P., Volkow, N. D., & Li, T. K. (2014). What if addiction is not a disease? The Lancet Psychiatry, 1(2), 105-107.
-
Popik, P., Layer, R. T., & Skolnick, P. (1995). 100 years of ibogaine: Neurochemical and pharmacological actions of a putative anti-addictive drug. Pharmacological Reviews, 47(2), 235-253.
-
Schenberg, E. E., Li, S. M., & Sanchez-Ramos, J. (2014). Ibogaine reduces behavioral and neurochemical effects of cocaine and methamphetamine. The Journal of Pharmacology and Experimental Therapeutics, 349(3), 424-432.
-
Swenson, E. (2009). The spirit of the forest: The Bwiti initiation into the secrets of the iboga plant. Journal of Religion in Africa, 39(3), 346-380.